The Spike Protein and Depression: Induction of the Depression Phenotype
Chronic inflammation induced by the Spike Protein is almost certainly the cause of Long COVID/Spike Injury depression.
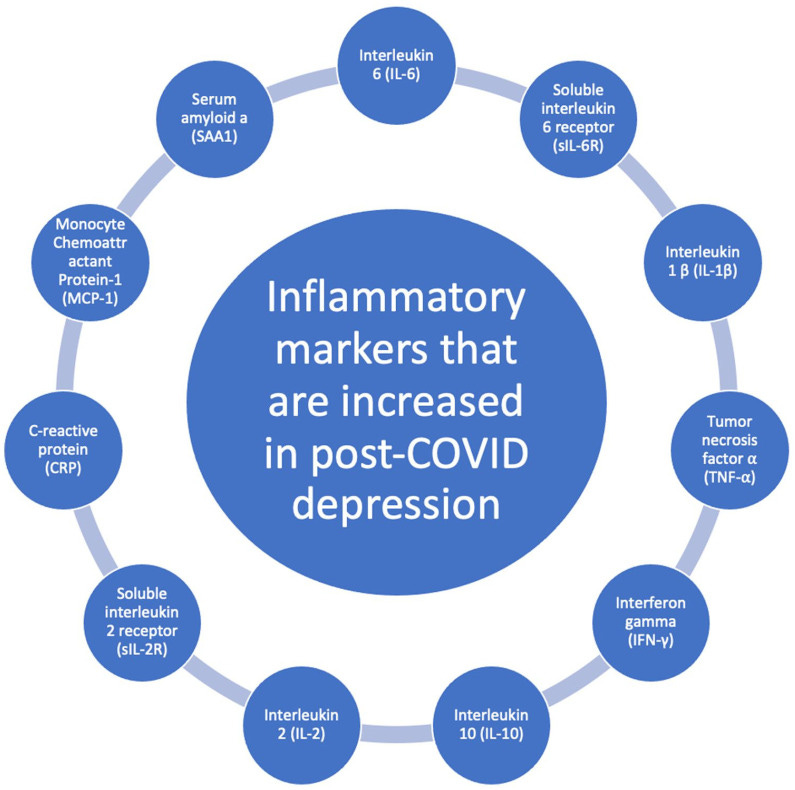
Role of inflammatory markers in post-COVID depression.
One of the most common symptoms experienced in Long COVID and Spike Protein injury is depression.
A meta-analysis of 51 studies included 18,917 patients with COVID-19 found that the most common neuropsychiatric PASC symptoms were insomnia (27%), fatigue (24%), cognitive deterioration (20%), anxiety (19%), post-traumatic stress disorder (PTSD; 15%), and depression (12.9%).
The Relationship Between COVID-19 and the Development of Depression: Implications on Mental Health
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10441207/
Yet, if we look at the totality of neuropsychiatric Long COVID symptoms we begin to see a picture emerge, and that is the picture of inflammation-induced depression. It is best to begin with a now well-established fact: The Spike Persists and Circulates in Those with Long COVID/Spike Injury.
This study, in agreement with other published investigations, demonstrates that both natural and vaccine spike protein may still be present in long-COVID patients, thus supporting the existence of a possible mechanism that causes the persistence of spike protein in the human body for much longer than predicted by early studies. According to these results, all patients with long-COVID syndrome should be analyzed for the presence of vaccinal and viral spike protein.
Presence of viral spike protein and vaccinal spike protein in the blood serum of patients with long-COVID syndrome
https://www.europeanreview.org/article/34685
Please note that the “Editor in Chief” of the publication retracted the above reference article. Please also note that its authors strongly disagreed with said retraction...
Additionally, if we look at the constellation of symptoms associated with Long COVID/Spike Injury depression, we notice that they are part of a phenotype known as the depression phenotype. The expression of the cytokines associated with the presence of the Spike Protein are precisely the cytokines which can either worsen or induce the depression phenotype.
The main aims of this paper are to explain how the various inflammatory and CMI pathways as well as their sequels and concomitants contribute to the pathophysiology of unipolar depression and may be associated with the onset of depression; and how all those factors act in concert to cause the neuroprogressive aberrations described in depression. Towards this end we will briefly review the CMI and inflammatory findings in clinical depression and the body of evidence that CMI activation, including increased production of interferon-γ (IFNγ) and interleukin-2 (IL-2); and pro-inflammatory cytokines (PICs), such as IL-1β, IL-6 and tumor necrosis factor-α (TNFα), may cause depressive-like behaviors, including melancholic symptoms (anhedonia); anxiety; fatigue and somatic symptoms; and neurocognitive symptoms as well. The symptomatology of human depression is indeed very complex and consists of different, albeit overlapping symptom dimensions: (a) the melancholic dimension, characterized by a distinct quality of depressed mood (anhedonia), non-reactivity, early morning awakening, anorexia, body weight loss, and cognitive and psychomotor disturbances; (b) the anxiety dimension, with tension, anxious behavior, and respiratory, genito-urinary and autonomic symptoms; (c) the fatigue and somatic dimension, with aches and pain, muscular tension, fatigue, concentration difficulties, failing memory, irritability, irritable bowel, headache, and a flu-like malaise; and (d) neurocognitive disorders, including mild cognitive impairment (MCI) (Maes, 2009).
Mechanistic explanations how cell-mediated immune activation, inflammation and oxidative and nitrosative stress pathways and their sequels and concomitants play a role in the pathophysiology of unipolar depression
https://www.sciencedirect.com/science/article/abs/pii/S0149763411002120
One possible therapeutic to treat this depression phenotype may be serotonin reuptake inhibitors.
Twenty-two studies fulfilled these criteria. Meta-analysis of these studies showed that, overall, while pharmacological antidepressant treatment reduced depressive symptoms, it did not reduce serum levels of TNFα. On the other hand, antidepressant treatment did reduce levels of IL-1β and possibly those of IL-6. Stratified subgroup analysis by class of antidepressant indicated that serotonin reuptake inhibitors may reduce levels of IL-6 and TNFα. Other antidepressants, while efficacious for depressive symptoms, did not appear to reduce cytokine levels. These results argue against the notion that resolution of a depressive episode is associated with normalization of levels of circulating inflammatory cytokines; however, the results are consistent with the possibility that inflammatory cytokines contribute to depressive symptoms and that antidepressants block the effects of inflammatory cytokines on the brain.
The Effect of Antidepressant Medication Treatment on Serum Levels of Inflammatory Cytokines: A Meta-Analysis
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3194072/
There is evidence that using SSRIs (selective serotonin reuptake inhibitors) does, indeed, ameliorate the depression phenotype symptoms.
In this study, 95 PCS patients were treated with selective serotonin reuptake inhibitors (SSRIs). This study used an exploratory questionnaire and found that two-thirds of patients had a reasonably good to strong response on SSRIs, over a quarter of patients had moderate response, while 10% reported no response. Overall, patients experienced substantial improved well-being. Brainfog and sensory overload decreased most, followed by chronic fatigue and dysautonomia.
Treatment of 95 post-Covid patients with SSRIs
https://www.nature.com/articles/s41598-023-45072-9
One additional point. The authors of the paper discussing the relationship between COVID-19 and the development of depression made the following statement regarding cause:
The long-term prevalence of depressive symptoms in COVID-19 survivors may be due to the prolonged state of high inflammatory marker levels. 8 The patients who are most vulnerable to post-COVID depression are those who had a severe disease course, since they had the highest levels of the inflammatory factors.
The Relationship Between COVID-19 and the Development of Depression: Implications on Mental Health
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10441207/
It is disappointing, though unfortunately expected, that they did not call out and discuss the most obvious cause: The Spike Protein.
I will continue to investigate the effects of and therapeutics for the Spike Protein on mental health. Thank you to the growing numbers of new and loyal supporters. You allow me to extend the depths of my research. I will continue working for understanding and healing.



Many thanks for an informative and well researched article.
Depressed people are generally 1-2 degrees warmer than the general public--see Dr. Gerald Raison, MD, Psychopharmacologist, U of Wisconsin, Madison. He recommends saunas and sweat lodges. I forgot the name of his book. The relationship between temperature and depression goes back to about 1725.