Friday Hope: Thiamine (Vitamin B1): Improving Endothelial Function Post Spike Protein Exposure
Vitamin B1 reduces mortality and incidence of thrombosis in those with severe COVID.
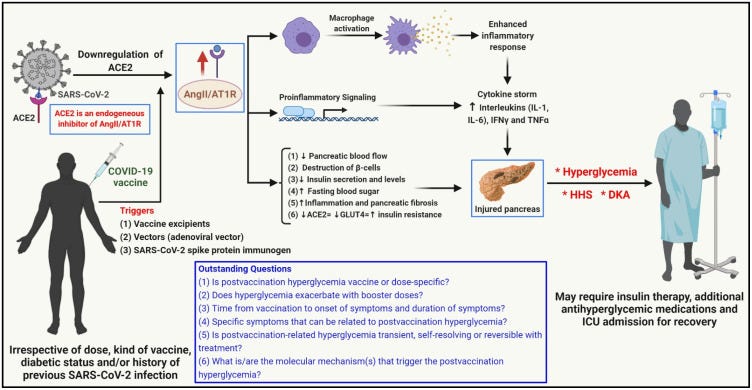
Possible mechanism of COVID-19 vaccination-associated pancreatic injury and hyperglycemia/hyperglycemic complications (figure adapted and modified from [7]). The angiotensin-converting enzyme 2 (ACE2) receptor, the key binding site for the SARS-CoV-2 virus, is a key regulator of the renin–angiotensin–aldosterone system (RAAS) and an endogenous inhibitor of the angiotensin II/angiotensin II type 1 receptor (AngII/AT1R) axis. SARS-CoV-2 binding to the pancreatic cells that express the ACE2 receptor and subsequent ACE2 downregulation diminish the inhibitory effect of ACE2 on the AngII/AT1R axis, which in turn leads to macrophage activation, upregulation of proinflammatory pathways, and hypercytokinemia (cytokine storm), culminating in pancreatic injury. It may be possible that vaccine excipients, vectors (adenoviral vectors), and the COVID-19 vaccine SARS-CoV-2 spike protein immunogen trigger similar mechanisms that cause pancreatic injury and subsequent hyperglycemia and hyperglycemic complications, such as hyperglycemic hyperosmolar syndrome (HHS) and diabetic ketoacidosis (DKA). Studies are warranted to address the outstanding questions in this area. Created with BioRender.com. * indicates potential postvaccination hyperglycemic scenarios.
As readers of this Substack are well aware, from the beginning I have hypothesized that the Spike Protein of SARS-CoV-2 causes what I have termed Spike Protein Endothelial Disease. Since then, numerous studies and papers have shown this to be the case. To that end, I believe one of the most important steps we can take to protect ourselves against the threat of the Spike Protein, and SARS-CoV-2 itself, is to protect our endothelium.
Vitamin B1 (Thiamine) may prove to be an invaluable resource in protecting the endothelium after Spike Protein exposure, or during the course of a COVID infection. Why? Because Thiamine protects the endothelium in the presence of hyperglycemia.
It is interesting (and not surprising) to note that both Spike Protein exposure and COVID infection induce hyperglycemia. This may be the critical factor in the observation that those who are Obese and those who have Diabetes fare far worse when infected with COVID.
Let’s first look at hyperglycemia and COVID infection.
Also expressed in the pancreas, ACE2 is crucial for maintaining glucose homeostasis. Insulin secretion is reduced, and islet cells are damaged as a result of COVID binding to ACE2 [20]. Contrarily, the COVID virus alters glucose tolerance and raises Blood Sugar by inducing Insulin Resistance and decreasing insulin release from the cells, which inhibits ACE2 and increases the synthesis of Ang II. Thus, it can be concluded that in patients with more severe COVID-19, the imbalance in the activity of AT1R and AT2R leads to metabolic disturbance, high BP, IR, and hyperglycemia.
A Review of Hyperglycemia in COVID-19
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10181889/
So, the infection produces a state of hyperglycemia. As I previously stated, it is not surprising that the Spike Protein (ACE2 reducer extraordinaire) alone induces hyperglycemia. Next, let’s look at the best Spike Protein producer we can find and its effects on Blood Sugar: The vaccines...
As mentioned earlier, acute pancreatitis and subsequent hyperglycemia or new onset of diabetes, owing to the direct or indirect cellular damage of the ACE2 receptor-expressing pancreatic islets, was reported in SARS-CoV-2-infected patients [4,7,8,9]. Apart from acting as a binding site for the SARS-CoV-2 virus, the ACE2 receptor is also responsible for maintaining the critical balance required for the proper functioning of the renin–angiotensin–aldosterone system (RAAS) [4,7]. However, the functional downregulation of the ACE2 receptor (due to viral binding and the resulting hyperactivation of the AngII/AT1R axis) triggers proinflammatory signaling mechanisms and macrophage activation in target organs, such as the pancreas [7]. The hypercytokinemia (cytokine storm) that follows the exaggerated inflammatory and immune response (1) decreases pancreatic blood flow, (2) impairs β-cell function, and (3) increases cellular oxidative stress, damaging the pancreas (fibrosis), causing a reduction in synthesis and secretion of insulin and a decrease in insulin sensitivity in target tissues, leading to the increase in blood glucose levels [4,7,10].
Interestingly, pancreatic injury/acute pancreatitis (in some cases recurrent pancreatitis) were reported in individuals following COVID-19 vaccine administration and could be a possible cause for postvaccination hyperglycemia in the affected individuals [16,17,18,19]. There is a possibility that inflammatory mechanisms (elevation of proinflammatory cytokines, such as IL-1, IL-6, IFNγ, and TNFα) in response to a trigger (such as vaccine excipients), the adenoviral vector (as in the case of the Covishield vaccine), or the SARS-CoV-2 spike protein immunogen (derived from the vaccine) may culminate in pancreatic endocrine system damage and subsequently in an acute hyperglycemic milieu.
COVID-19 Vaccines and Hyperglycemia—Is There a Need for Postvaccination Surveillance?
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8952286/
Now we arrive at the star of our show: Thiamine (Vitamin B1). As a therapeutic it addresses both conditions discussed, infection and Spike Protein exposure. Thiamine has proven useful in treating critical COVID. It should almost benefit all those suffering an acute infection.
A total of 738 critically ill patients with COVID-19 who had been admitted to ICUs were included in the study. Among 166 patients matched using the propensity score method, 83 had received thiamine as adjunctive therapy. There was significant association between thiamine use with in-hospital mortality (OR = 0.39; 95% CI 0.19–0.78; P value = 0.008) as well as the 30-day mortality (OR = 0.37; 95% CI 0.18–0.78; P value = 0.009). Moreover, patients who received thiamine as an adjunctive therapy were less likely to have thrombosis during ICU stay [OR (95% CI) 0.19 (0.04–0.88), P value = 0.03].
Conclusion
Thiamine use as adjunctive therapy may have potential survival benefits in critically ill patients with COVID-19. Additionally, it was associated with a lower incidence of thrombosis. Further interventional studies are required to confirm these findings.
Evaluation of thiamine as adjunctive therapy in COVID-19 critically ill patients: a two-center propensity score matched study
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8242279/
Moreover, Vitamin B1 has the ability to improve endothelial function in the presence of hyperglycemia. It may therefore ameliorate the endothelial damage done by the presence of the Spike Protein.
Brachial artery vasoactivity (BAVA) is a reliable, noninvasive method of assessing endotheliumdependent vasodilatation (EDV) in vivo. Acute hyperglycemia, impaired glucose tolerance (IGT), and diabetes mellitus impair EDV, a precursor to atherosclerosis. Thiamine is a coenzyme important in intracellular glucose metabolism. The purpose of this study was to evaluate the effect of thiamine on BAVA in the presence of hyperglycemia. Ten healthy subjects (group H, mean age 27 years), 10 patients with impaired glucose tolerance by World Health Organization criteria (group IGT, mean age 65 years), and 10 patients with non-insulin-dependent diabetes mellitus (group NIDDM, mean age 50 years) were studied. Duplex ultrasound was used to measure brachial artery flow changes in response to reactive hyperemia following brachial artery tourniquet occlusion for 5 min. This test was performed after a 10 hr fast and at 30, 60, and 120 min after a 75 g oral glucose challenge along with measurements of blood glucose level (BGL). A week later, BAVA evaluation was repeated after administration of 100 mg of intravenous thiamine. BAVA (% increased blood flow) at peak and trough BGL was compared with and without thiamine. BAVA at peak glucose improved from 69.0 ± 6.4% to 152.8 ± 22.9% in group H (p < 0.005), from 57.6 ± 12.6% to 139.7 ± 12.4% in group IGT (p < 0.005), and from 57.8 ± 8.3% to 167.8 ± 11.6% in group NIDDM (p < 0.005) following administration of thiamine. On the other hand, at trough glucose levels, BAVA remained essentially unchanged in group H (prethiamine 83.8 ± 6.5% vs. post-thiamine 83.8 ± 17.0%, p > 0.05) as well as group IGT (prethiamine 96.7 ± 8.5% vs. post-thiamine 104.0 ± 17.4%, p > 0.05). BAVA at trough glucose was not measured in group NIDDM secondary to trough BGL > 140 mg/dL. EDV was improved by thiamine in the presence of hyperglycemia in healthy subjects and in patients with IGT and NIDDM. The mechanism by which thiamine improves EDV is not due to a glucose-lowering effect as thiamine had no effect on EDV under normoglycemic conditions. Routine administration of thiamine might improve endothelial function and therefore slow the development and progression of atherosclerosis, especially in patients with IGT and NIDDM who are prone to develop accelerated atherosclerosis.
Thiamine (Vitamin B1) Improves Endothelium-Dependent Vasodilatation in the Presence of Hyperglycemia
https://www.annalsofvascularsurgery.com/article/S0890-5096(07)60182-4/abstract
It may be the case that Vitamin B1 can help those affected with Long COVID, due to presence of Spike Protein. I will research this potential benefit.
Once again, I thank everyone for their support, readership and dialog. Today is as good as it gets during a Vermont summer: An American Paradise. Eighty degrees, a light breeze, brilliant sunshine and low humidity. I wish for brilliant sunshine in all our lives this weekend. Blessings and hope to all.



There are more effective forms of Thiamine perhaps Benfotiamine...
And yes from personal experience and from anecdotal acounts i have seen it might help some forms of LC.
Thank you Walter for bringing Thiamine to your reader's attention. Thiamine, especially as Thiamine TTFD ( Allithiamine) and Benfotiamine has very interesting metabolic effects. There is important research by Constantini and Lonsdale which EO Nutrition on YouTube goes into great detail about. Thiamine is an important component of mitochondrial production of energy and stage one of the electron transport chain as well as being crucial for glucose metabolism. High dose Thiamine has been used for Parkinson's and other neurological diseases, sleep apnea, diabetes, and as Walter mentions, seems promising for Long COVID. Note the effect on methylation and understand the so-called "paradoxical effect" before mega dosing ...