Ronca, et al. Provide Hints That Long COVID May Be a Novel Systemic Autoimmune Disease
Looking at patients with excess weight, the review notes persistent symptoms shared with Rheumatoid Conditions and MS.
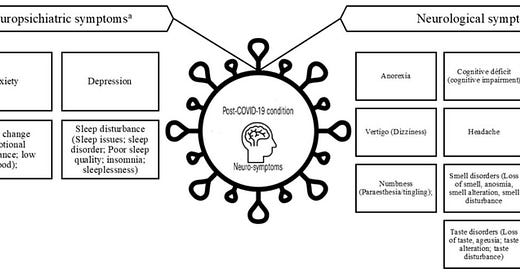
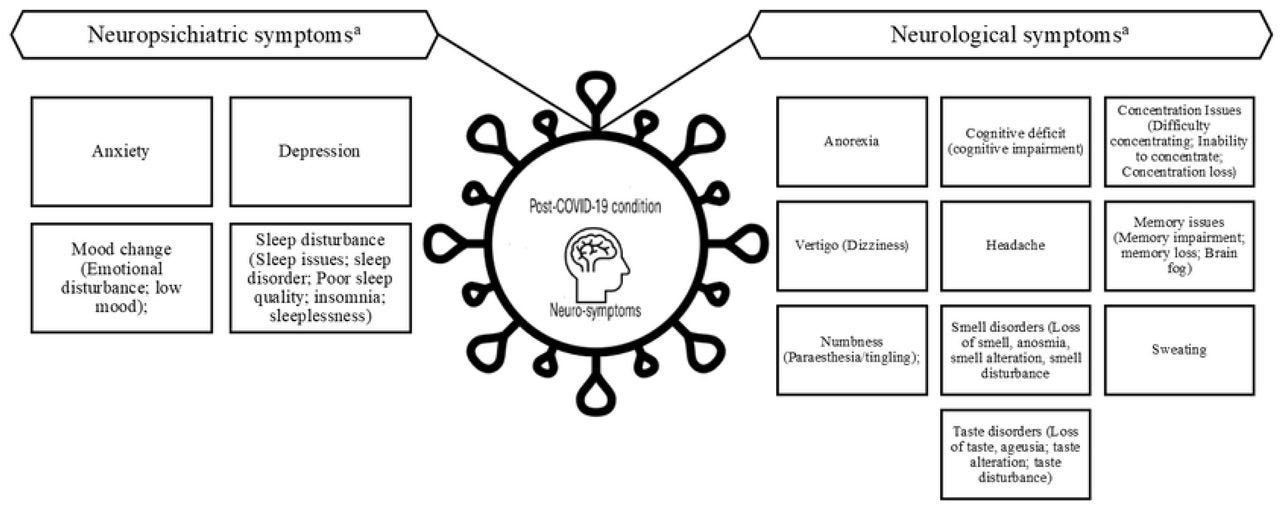
Reported neurological and neuropsychiatric symptoms related to Post-COVID-19 condition (PCC)
A pre-print published online last Wednesday revealed some very interesting information. In patients with excess weight who were experiencing Long COVID, some neuropsychiatric symptoms were heavily shared between them.
Although it has been suggested that individuals with increased BMI are at higher risk of PCC (Post COVID Condition), the associations between EW (Excess Weight) and specific PCC related neurological and neuropsychiatric symptoms remained unclear. Our review reveals that EW is significantly associated with a range of persistent and PCC symptoms, including headache, vertigo, smell and taste disorder, sleep disturbance and depression.
Excess weight increases the risk for neurological and neuropsychiatric symptoms in post-COVID-19 condition: A systematic review and meta-analysis
https://www.medrxiv.org/content/10.1101/2024.11.20.24317635v1.full
It was this particular constellation of symptoms that caught my attention. If we look at autoimmune disease, we find these to be very common symptoms – and being obese can be an aggravating and/or initiating factor.
First, rheumatoid conditions.
This study included only individuals with RA, but high levels of fatigue have been found in other rheumatic conditions, including osteoarthritis, systemic lupus erythematosus, psoriatic arthritis, and ankylosing spondylitis [52–57]. Relatively high prevalence rates of obesity, depression, sleep disturbance, and/or inactivity have been reported each of these conditions [58–63], so it is possible that these factors may play an important role in fatigue in other rheumatic conditions. In fibromyalgia, another condition with high levels of fatigue, sleep disturbances, depression, obesity, and inactivity are common[64,65]. In fact, physical activity or exercise interventions have been identified as effective interventions for fibromyalgia symptoms[66].
The Role of Sleep Disturbance, Depression, Obesity, and Physical Inactivity in Fatigue in Rheumatoid Arthritis
https://pmc.ncbi.nlm.nih.gov/articles/PMC6083443/
Now, many of these very same symptoms are also intimately related with a different type of autoimmune disease: Multiple Sclerosis.
The symptoms of multiple sclerosis (MS) vary greatly from person to person, and can get better or worse over time. More common symptoms include fatigue, walking (gait) difficulties, numbness or tingling, spasticity, weakness, vision problems, dizziness, bladder and bowel problems, sexual problems, pain, cognitive and emotional changes, and depression.
9 Unusual Symptoms of Multiple Sclerosis (MS)
https://www.everydayhealth.com/multiple-sclerosis/symptoms/the-most-surprising-symptoms-of-multiple-sclerosis/
The article goes on to discuss additional, lesser known symptoms of MS, such as those reported in the review: Vertigo, Headache and Smell and Taste Disorder.
Now we arrive at the point. It is not so much that SARS-CoV-2 is inducing RA or MS. It is that it appears to be inducing an altogether novel form of autoimmune disease. For, RA and MS themselves are intertwined.
A total of 1456 newly diagnosed patients with MS and 10,362 control patients were matched for age, sex, and initial diagnosis date. Patients with MS had a higher incidence of rheumatoid arthritis (age-adjusted standardized incidence ratio: 1.72; 95% confidence interval = 1.01–2.91). There was a positive correlation in being diagnosed with rheumatoid arthritis in patients previously diagnosed with MS when stratified by sex and age. The strength of this association remained statistically significant after adjusting for sex, age, and smoking history (hazard ratio: 1.78, 95% confidence interval = 1.24–2.56, P = 0.002).
In conclusion, this study demonstrates that a diagnosis of MS increased the likelihood of a subsequent diagnosis of rheumatoid arthritis in patients, independent of sex, age, and smoking history.
Increased incidence of rheumatoid arthritis in multiple sclerosis
https://pmc.ncbi.nlm.nih.gov/articles/PMC4937922/
Obesity just makes things worse.
Results Presence of obesity at disease onset was associated with higher disability at baseline and at 2, 4 and 6 years of follow-up (p<0.001). Median time to reach EDSS 3 was 0.99 years for patients with BMI ≥30 kg/m2 and 1.46 years for non-obese patients. Risk to reach EDSS 3 over 6 years was significantly increased in patients with BMI ≥30 kg/m2 compared with patients with BMI <30 kg/m2 after adjustment for sex, age, smoking (HR 1.87; 95% CI 1.3 to 2.6; log-rank test p<0.001) and independent of disease-modifying therapies. Obesity was not significantly associated with higher relapse rates, increased number of contrast-enhancing MRI lesions or higher MRI T2 lesion burden over 6 years of follow-up.
Conclusions Obesity in newly diagnosed patients with MS is associated with higher disease severity and poorer outcome. Obesity management could improve clinical outcome of MS.
Association of obesity with disease outcome in multiple sclerosis
https://jnnp.bmj.com/content/94/1/57
My takeaway? I see a “conveyor belt” effect. Let’s say Spike Protein Autoimmune Disease is ten miles down the road for a young, healthy individual. (Bear in mind, we are all on this road). Now, Obesity puts you three miles further down the road, nearer that ten mile marker. Old age may put you eight miles down the road. Becoming exposed to the Spike Protein may put you an additional mile or two down the road.
Do you see the concern?
It’s not so much, perhaps, that the old and obese are likely to suffer more from SARS-CoV-2 and its Spike Protein, it’s that they are already further along the path of destruction the virus and its proteins cause. So, they are swept faster into its maelstrom. Those of us who are younger and healthier may feel immune. Yet, each exposure to the Spike Protein, each SARS-CoV-2 infection, pushes us further down that road others had a “head start” on. Indeed, evidence abounds supporting my very early hypothesis that SARS-CoV-2 and its Spike Protein accelerate aging.
I will continue to search for understanding and solutions. Happiest of Thanksgivings to those in America! Blessings to all! I am profoundly Thankful for your readership, dialog and support, as always.


Long Covid is caused by chronic oxidative stress & depletion of glutathione and essential minerals from the injected vaccine ingredients.
Repletion of glutathione & zinc, selenium, magnesium etc ends long Covid.
Monthly parasite cleanses + heavy metals chelation via Emeramide aka OSR / NBMI, which OSR = Oxidative Stress Reduction (raises blood / brain glutathione levels more than anything on the planet) and crosses the blood / brain barrier inactivating mercury, lead, cadmium, etc. the toxic heavy metals that IMHO are the source of the symptoms that present as autoimmune, MS, neuropathies, long covid, etc.