BREAKTHROUGH: The Endothelial Phase (SPED) of Spike Protein Amyloid Deposition Disease is Just the Beginning: The Dangers of Reinfection
A disease of the Extracellular Matrix (ECM)? Looking carefully, we discover that the Spike Protein is a signaling protein which travels from the Endothelium to the ECM, where it proceeds to lay waste.
This is my most important Substack post to date.
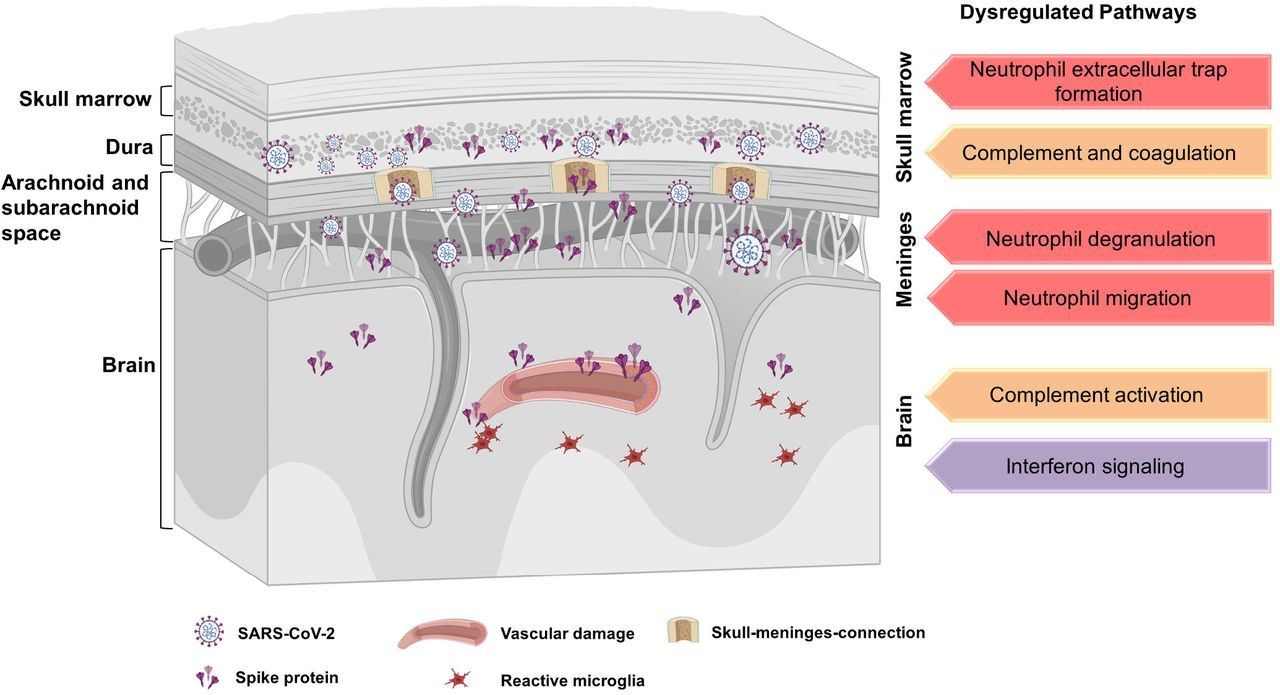
The above image is the best representation I could find of what I believe the Spike Protein induces AFTER it has attacked the Endothelium causing what I have called Spike Protein Endothelial Disease (SPED). Please see my previous posts on this subject for an explanation. However, if you have not yet read them, general knowledge of what the Spike Protein does to the vasculature should be more than sufficient to give you an idea.
I now propose that SPED is but the first step in a disease process which is, ultimately, a disease of the Extracellular Matrix. A disease where the Spike Protein invades the extracellular matrix via the Endothelium and then precipitates amyloids systemically, throughout all major organs and systems.
Sometimes it is a secondary, seemingly innocuous point that we read which becomes the springboard to major discoveries. Let’s look at two passages from a paper published just over two weeks ago which set off a vast array of lightbulbs in my mind.
We studied whether amyloid-containing deposits were present in the skeletal muscle of long COVID patients and whether the indication of post-exertional malaise changed the concentration. We demonstrate that the concentration of amyloid-containing deposits was greater in the skeletal muscle of long COVID patients at baseline, and increased similarly in both groups after the induction of post-exertional malaise
Visualizing amyloid-containing deposits together with capillaries or lymph vessels revealed that the skeletal amyloid-containing deposits were not located in capillaries or lymphatic vessels, but rather next to capillaries and in the extracellular matrix between muscle fibers.
Muscle abnormalities worsen after post-exertional malaise in long COVID
https://www.nature.com/articles/s41467-023-44432-3
If we look back to 2015, we find a paper which demonstrates that it is within the extracellular matrix that amyloids precipitate.
Amyloidosis is a group of protein misfolding disorders in which normal circulating proteins misfold and self-aggregate into fibrillar polymers that precipitate in the extracellular space [1]. The disease can be systemic when several organs and connective tissue matrix are widely involved, or localized if only a single anatomical site or organ system is affected. In many cases of systemic amyloidosis, amyloid deposition is most prominent in specific organs, such as the liver, the heart, the spleen or the nerves, and this dictates the specific clinical features. Although there is clinical and experimental evidence suggesting that some specific constituents of the extracellular matrix (ECM), such as proteoglycans may play a crucial role in determining the specificity of tissue localization of amyloid deposits [2], accurate analysis of the interaction between amyloid and the biochemical and biophysical structure of the ECM has been so far been limited by technical factors.
Here, we report in mice with transgenic overexpression of mouse amyloid A (AA) [12] that hepatic AA amyloid deposits [12] persisted in the ECM after complete decellularization of the liver. The primary structure of the amyloid fibril protein was unaffected by the procedure and amyloid extracted from decellularized liver retained the amyloid enhancing factor (AEF) property that accelerates, in vivo, AA amyloid formation. In addition, scanning electron microscope (SEM) images of the scaffold of the decellularized amyloidotic organ provided a unique 3D visualization of the intimate relationship between the amyloid fibrils and the ECM network.
Amyloid persistence in decellularized liver: biochemical and histopathological characterization
https://pmc.ncbi.nlm.nih.gov/articles/PMC4819572/
Now, let’s remind ourselves that the Spike Protein is amyloidogenic and those with COVID see a dramatic increase in Serum Amyloid A (SAA). This is also, and very importantly, true for those suffering from Long COVID.
SAA was also significantly upregulated in our Long COVID samples. SAA contains binding sites for the extracellular matrix components, laminin and heparin/heparan sulfate, as well as the RGD-like (arginine-glycine aspartic acid) adhesion motif (58). Immobilized SAA also binds to the αIIbβ3 receptor on platelets (58) and may also directly bind to toll-like receptors (TLR) on endothelial cells (68). Dysregulated SAA is associated with endothelial dysfunction and early-stage atherogenesis (69). SAA binding to on endothelial cells results these cells express ICAM-1, VCAM-1, E-selectin, TNF-α, IL-1, and IL-6, together with pro-thrombotic factors (68) (see Figure 7).
Increased levels of inflammatory molecules in blood of Long COVID patients point to thrombotic endotheliitis
https://www.medrxiv.org/content/10.1101/2022.10.13.22281055v1.full
Once we are aware of this mechanism, the evidence that the Spike Protein is invading the extracellular matrix and inducing systemic amyloidosis is everywhere. How do we know it is the Spike? Results from transfection.
Shahandeh et al. [62] (see Table 2) reported a 54-year-old woman with a background of recent non-ischemic cardiomyopathy attributed to COVID-19 vaccination-induced myocarditis presenting with cardiogenic shock. She received mechanical circulatory support followed by uncomplicated heart transplantation. The explanted heart pathology confirmed a diagnosis of kappa AL amyloidosis.
There was also one other case of cardiac amyloidosis which appears to have developed following COVID-19 vaccination, though this was diagnosed upon post-mortem examination. Hansen et al. [63] made a histological diagnosis of cardiac amyloidosis in a previously well and symptomless 86-year-old man who died following a single dose of mRNA Pfizer-BioNTech COVID-19 vaccination.
COVID-19 Infection and Vaccination and Its Relation to Amyloidosis: What Do We Know Currently?
https://pmc.ncbi.nlm.nih.gov/articles/PMC10383215/
What concerns me even more, is that the induction of Amyloidosis may happen upon reinfection. Readers may recall several of my posts on X, where I refer to the SARS-CoV-2 as the battering ram Grond from LOTR. It will continue to break down our defenses until we finally submit. This, I believe, is the ultimate battle we face with the Spike Protein. There is also the concern that it retrotranscribes and is continually expressed within our bodies. This is still under investigation.
A case demonstrating induction of Amyloidosis upon reinfection.
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection has been associated with the overproduction of serum amyloid A protein, resulting in systemic AA amyloidosis. In this report, we describe a case of gastrointestinal (GI) AA amyloidosis following SARS-CoV-2 infection. A 75-year-old male presented to the emergency department with upper abdominal pain 6 weeks post kidney transplantation. He had a history of SARS-CoV-2 infection 4 weeks prior. On day 7 of hospitalization, while receiving conservative management, the patient developed symptoms of cough and fever, leading to a diagnosis of SARS-CoV-2 reinfection. The patient’s abdominal pain persisted, and hematochezia developed on day 30 of hospitalization. Esophagogastroduodenoscopy and colonoscopy revealed multiple ulcers in the stomach and colon, with histologic findings revealing the presence of amyloid A. The patient was managed conservatively and was also given remdesivir for the SARS-CoV-2 infection. His clinical symptoms subsequently improved, and endoscopic findings demonstrated improvement in multiple gastric ulcers. GI amyloidosis may be a subacute complication following SARS-CoV-2 infection in immunocompromised patients.
Gastrointestinal AA Amyloidosis following Recurrent SARS-CoV-2 Infection: A Case Report
https://pmc.ncbi.nlm.nih.gov/articles/PMC10375246/
We have many tools with which to fight this. However, I am extremely concerned about exposure to the Spike Protein, in any form, over time. Transfection appears to be a bullet train to Spike Protein exposure.
It is my hope that clinicians will screen their patients suffering from Long COVID for Amyloidosis. In fact, I believe all of us (the general population) should be screened for the presence of Amyloidosis and levels of Sereum Amyloid A, so we may ascertain the scale of this dilemma.
Thank you, as always, for your readership, dialogue and support. I will continue to investigate and report back to you.



Could you do an interview with Kevin McCairn discussing this latest discovery by you?
No way out? Such is life.
But there is a way out, ultimately.
“Jesus said to him, ‘I am the way, the truth, and the life. No one comes to the Father except through Me.’”
John 14:6