An Explanation for Observed SARS-CoV-2 Seizures and why Antibodies Post Exposure May be Severely Damaging the Brain
Blood Brain Barrier disruption and IgG leakage may be a major driving force of COVID neurological pathology.
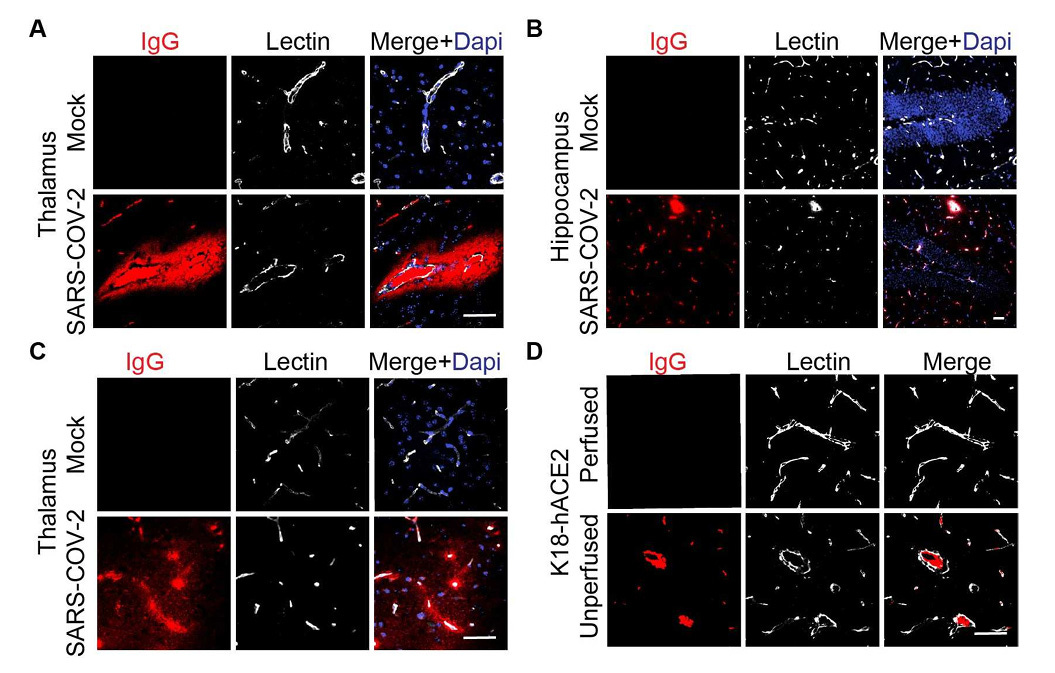
Additional data on vascular damage and potential BBB breakdown in SARS-CoV-2 infected K18-hACE2 model. (A) Representative images of immunofluorescent IgG staining showing microhemorrhage in the thalamus area of K18-hACE2 mice. Bar: 50 µm. (B-C) Representative images showing immunofluorescent staining for IgG at the capillary level in the hippocampus and thalamus areas. Bar: 50 µm. (D) Representative images showing IgG immunofluorescent staining in the cortex of perfused or unperfused mouse. Bar: 50 µm.
A preprint published February 10th of this year confirms an aspect of SARS-CoV-2 infection that I have been writing about for years. That is Blood-Brain Barrier infiltration and vascular inflammation. One finding which the authors did not discuss, but which I will, is the extravasation of IgG in the brain.
Our study further indicated that the structural changes in cerebral microvessels and BBB are key pathological phenomenon during SARS-CoV-2 infection in the K18-hACE2 infection model. We reported a notable rise in the occurrence of microhemorrhages in the mouse brain infected with SARS-CoV-2. In areas without microhemorrhages, we also noted a substantial increase in IgG extravasation, particularly in the cortex, thalamus, and hippocampus. This underscores the significant impact of SARS-CoV-2 on microhemorrhages and emphasizes its impact on BBB integrity. Nevertheless, the current research remains limited on this direction, and future studies are still urgently needed to explore the fundamental biology in models with mild infection and long-COVID scenarios, and determine to what extent the breakdown of the brain barriers may contribute to the neurological complication in the development of PASC.
SARS-COV-2 induces blood-brain barrier and choroid plexus barrier impairments and vascular inflammation in mice
https://www.biorxiv.org/content/10.1101/2024.02.09.579589v1.full.pdf
Why is this so important? Because IgG extravasation may be the reason why individuals suffer from seizures either during Acute COVID or in PASC. It may also contribute to the development of neurodegenerative conditions associated post COVID infection.
Focal epilepsies are often associated with blood-brain barrier disruption. In 4 entorhinal cortex tissue samples and 13 hippocampal samples from patients with pharmacoresistent temporal lobe epilepsy, we observed immunoglobulin G (IgG) leakage in the parenchyma and IgG-positive neurons that had evidence of neurodegeneration, such as shrinkage and eosinophilia.
IgG Leakage May Contribute to Neuronal Dysfunction in Drug-Refractory Epilepsies With Blood-Brain Barrier Disruption
https://academic.oup.com/jnen/article/71/9/826/2917548
Detection of blood-brain barrier leakage in AD patients goes back to the 1980s when researchers discovered serum-borne proteins such as IgG and albumin in the brain parenchyma, indicating a compromised blood-brain barrier in AD patients (Alafuzoff, Adolfsson, Bucht, & Winblad, 1983; Alafuzoff, Adolfsson, Grundke-Iqbal, & Winblad, 1987). Although the idea that barrier leakage could play a role in AD pathology was controversial for decades, recent clinical data emphasizes a link between barrier leakage and cognitive decline in AD patients. In the following section, we will summarize the studies that identified barrier leakage in AD.
Blood-brain barrier leakage in Alzheimer’s disease: From discovery to clinical relevance
https://www.sciencedirect.com/science/article/pii/S0163725822000134
Indeed, as with so much SARS-CoV-2 and Spike Protein, it is a condition of aging.
Aged mice also have hallmarks of BBB breakdown compared to young mice with increased leakage of IgG into the brain parenchyma, a reduction of the tight junction protein occludin, and a reduction in pericyte coverage and pericyte induced expression of genes in the endothelium.
The blood-brain barrier in aging and neurodegeneration
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9156404/
One other concern: The levels of IgG post COVID vaccination. The antibody load itself may be causing/exacerbating neurodegeneration. Please note this third dose evidence:
The median level of IgG antibodies was 4.65 times higher at 10–12 weeks after the third dose of the vaccine in comparison to 25 weeks after the second dose of the vaccine. The next two measurements revealed also similar, statistically significantly higher IgG levels than the first one.
The Levels of Anti-SARS-CoV-2 Spike Protein IgG Antibodies Before and After the Third Dose of Vaccination Against COVID-19
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9843475/
The above may also explain why some experience more severe cases of COVID if infected weeks after mRNA.
I will work on discovering protocols to not only reduce Spike load, but also enhance BBB integrity. Thank you, as always, for your support, readership and dialog.



From correlation we proceed to causation. Great work and another piece of the jigsaw although endotoxins may also have a role to play. Big thanks from all the little people, we live and learn.
I saw this story in my local paper this evening:
'Healthy woman dies of sudden unexplained seizure
Stacey Harris, from Cardiff, was just 30 years old
The inquest was told 10 months before her death Mrs Harris had collapsed while brushing her teeth but came around quickly and did not have other symptoms of an epileptic fit. Other than this she had no relevant medical history and was described as “perfectly healthy” by her mother.
There was no history of allergies or anaphylaxis in her family. Her maternal grandfather died of a heart attack and her paternal grandfather had a pacemaker fitted with her father having a stent installed in recent years. Her mother has been diagnosed with epilepsy in her 50s after a 12-year history of symptoms.
Mrs Harris had Covid a short time before her death and tested negative on December 17. A toxicology report found no drugs in her system and an amount of alcohol the coroner said was not significant.
Pathologist Dr David Hywel Thomas and his colleagues conducted a post-mortem examination. From this and the evidence he heard he outlined two likely options which were that Mrs Harris suffered a seizure either due to epilepsy or heart arrhythmia, which can be passed on genetically. He could not conclude which was more likely on the balance of probabilities.
The coroner, Rachel Knight, considered the facts and recorded the medical cause of death as “sudden death due to seizure of unknown etiology (medical causes) resulting in a hypoxic brain injury.” Ms Knight reached a conclusion that Mrs Harris’ death was due to natural causes.'
Full article:
https://www.walesonline.co.uk/news/wales-news/healthy-woman-dies-sudden-unexplained-28622877