All Roads Lead From SPED: Cancer, Fibrosis and Neurodegeneration All Induced By SPED
Previous tissue injury is required for tumor emergence. – Rudolf Virchow, 1863
As I continue to search for a unifying pathology for COVID, Long COVID and SPED, I believe I am now even more on target. Given that the Spike Protein has been found to be circulating in those with Long COVID, and that the Spike Protein is responsible for constant endothelial injury, I believe that it is this mechanism which can induce the CHRONIC phase of SPED, which is the induction of cancer, fibrosis and neurodegeneration.
CANCER
First, let us examine how SPED may induce cancer, as this mechanism can explain why we are seeing such an abundance of cancer, and of very diverse types. I will now quote from a superb article, which I recommend all to read.
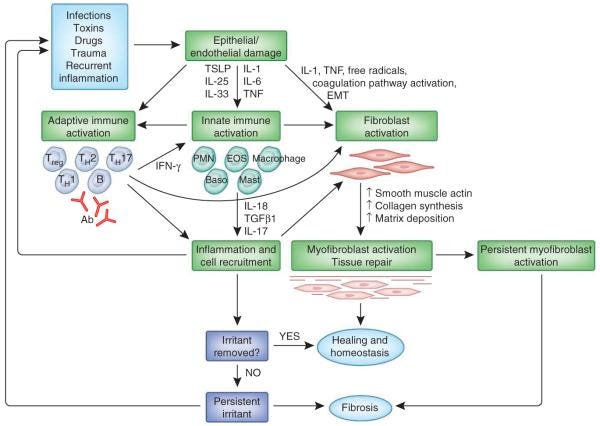
Can the prevalence of inflammation be the link between tissue injury and cancer? Recent studies have highlighted the particular importance of inflammation in both processes. These studies have indicated that the role of inflammation extends far beyond protection of the injured tissue from infectious agents and removal of damaged cells. In fact, inflammation is critical to almost every phase of tissue repair and tumorigenesis. Thus, we put forth that injury causes inflammation, which in turn orchestrates wound healing and tissue regeneration. If the inflammation cannot be resolved or is chronically provoked by repetitive injury or other factors, the resulting unchecked wound healing process can promote cancer formation. This hypothesis is supported by a large body of data, which is briefly summarized below and depicted in Figure 1 (above).
Several studies have implicated inflammation in stem cell function. For example, cytokines such as TNF and IL-6 promote stem cell proliferation (Widera et al., 2006), and their transcriptional effectors NF-κB and STAT3 are involved in stem cell renewal (Matsuda et al., 1999) and cancer (Grivennikov et al., 2010). Much emphasis has recently been placed on cancer stem cells (CSC), the functional homologs of somatic stem cells that are responsible for tumor initiation and regrowth after debulking (Lobo et al., 2007). While still poorly explored, inflammation is likely to promote CSC maintenance and proliferation. Reactive oxygen species (ROS), possibly originating from inflammatory cells, can modulate self-renewal of chronic myeloid leukemia stem cells (Miyamoto et al., 2007). Furthermore, macrophages can promote CSC tumorigenicity through IL-6, STAT3 and the Hedgehog pathway (Jinushi et al., 2011) and IL-6, STAT3 and NF-κB can convert non-stem cells to CSC (Iliopoulos et al., 2011). These findings lend support to the idea that cancer and wound healing progress through similar mechanisms, many of which are affected by inflammatory cytokines.
Chronic tissue damage and inflammation have long been suspected for their ability to promote cancer development and progression, but only recently was the incriminating “smoking gun” identified through the extensive use of physiologically relevant mouse models. Importantly, the experimental evidence obtained in mice is strongly supported by correlative and retrospective analysis of human clinical and epidemiological data. One of the earliest experiments that underscored the importance of tissue injury and cell death in tumorigenesis was the demonstration that v-Src cannot induce cancer unless accompanied by tissue injury and subsequent regeneration (Sieweke et al., 1990).
Taken together, these and many other experiments illustrate the pro-tumorigenic activity of cell death and together with clinical and epidemiological findings support the notion that a substantial fraction of all cancer cases are likely to be initiated and promoted by chronic tissue injury (Figure 3, above). These conclusions also suggest that therapeutic approaches that minimize injury and restore normal tissue homeostasis can be used in cancer prevention.
Tumor Promotion via Injury- and Death-induced Inflammation
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3587290/
FIBROSIS
This same mechanism, repeated injury, also induces fibrosis. Again, another superb article recommended for reading.
Fibrosis is a pathological feature of most chronic inflammatory diseases. Fibrosis, or scarring, is defined by the accumulation of excess extracellular matrix components. If highly progressive, the fibrotic process eventually leads to organ malfunction and death. Fibrosis affects nearly every tissue in the body. Here we discuss how key components of the innate and adaptive immune response contribute to the pathogenesis of fibrosis.
Fibrosis is the final, common pathological outcome of many chronic inflammatory diseases. Although collagen deposition is an indispensable and, typically, reversible part of wound healing, normal tissue repair can evolve into a progressively irreversible fibrotic response if the tissue injury is severe or repetitive or if the wound-healing response itself becomes dysregulated.
And, this is related to ENDOTHELIAL DAMAGE!
Epithelial and/or endothelial damage caused by various insults triggers complex interconnected wound-healing programs to quickly restore homeostasis. Failure to adequately contain or eliminate the inciting factors can exacerbate the inflammatory response and lead to a chronic wound-healing response, with continued tissue damage, repair and regeneration, ultimately resulting in fibrosis.
Mechanisms of fibrosis: therapeutic translation for fibrotic disease
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3405917/
NEURODEGENERATION
Normalized (Z-scored) neuropsychological performance of groups with mild traumatic brain injury (TBI; 1 mild TBI, n = 29; >1 mild TBI, n = 14) relative to control subjects (mean for control subjects, 0.0). Shaded box represents 1 standard deviation around the control mean. A, attention; E, executive function; M, memory.
Finally, we can now explain how SPED is also responsible for the observed abundance of emerging neurodegenerative diseases. Interestingly, we can learn about this mechanism by studying those who have been injured in the military. Though, perhaps, a milder form of Traumatic Brain Injury (TBI), it is certainly clear that COVID (including the microvascular damage of SPED) mimics the effects of TBI.
These results demonstrate that brain injury is a common consequence of both COVID-19 and influenza, and is therefore likely to be a feature of severe viral infection more broadly. The brain injury occurs in the context of dysregulation of both innate and adaptive immune responses, with no single pathogenic mechanism clearly responsible.
Brain injury in COVID-19 is associated with dysregulated innate and adaptive immune responses
https://academic.oup.com/brain/article/145/11/4097/6692467
One more excellent paper can explain how the brain damage from SPED is responsible for the observed dramatic increase in neurodegenerative diseases.
Population-based studies have supported the hypothesis that a positive history of traumatic brain injury (TBI) is associated with an increased incidence of neurological disease and psychiatric comorbidities, including chronic traumatic encephalopathy, Alzheimer's disease, Parkinson's disease, and amyotrophic lateral sclerosis. Key factors that likely mediate the degree of risk of neurodegeneration include genetic factors, significant premorbid and comorbid medical history (e.g. depression, multiple head injuries and repetitive subconcussive impact to the brain, occupational risk, age at injury, and severity of brain injury).
Imaging chronic traumatic brain injury as a risk factor for neurodegeneration
https://www.sciencedirect.com/science/article/pii/S1552526014001307
As the above figure demonstrates, the more injuries received, the greater the deficits. Though this may seem to be glaringly obvious, it is important to consider that constant presence of the Spike Protein would almost certainly mean constant endothelial damage, Of course, in the context of the brain, this would necessarily be constant brain injury.
I hope this essay will help develop a deeper understanding of how SPED may indeed be the lion’s share of COVID and Long COVID. I will keep searching for therapeutics. The question of Spike Protein persistence, reexposure and reinfection are constantly on my mind. Is there a limit to the protein’s damage? Is it ever increasing? Is it relapsing/remitting? Once initiated, can it be cured? These and many other questions I will endeavor to answer for all of us.
Thank you for your support. As always, I will continue to work.







This is first-rate research, Walter, truly brilliant! I've not seen anyone do a better job of putting these pieces together into such a comprehensive whole.
Amazing work Walter. I hope people are reaching out to you to tap your expertise.